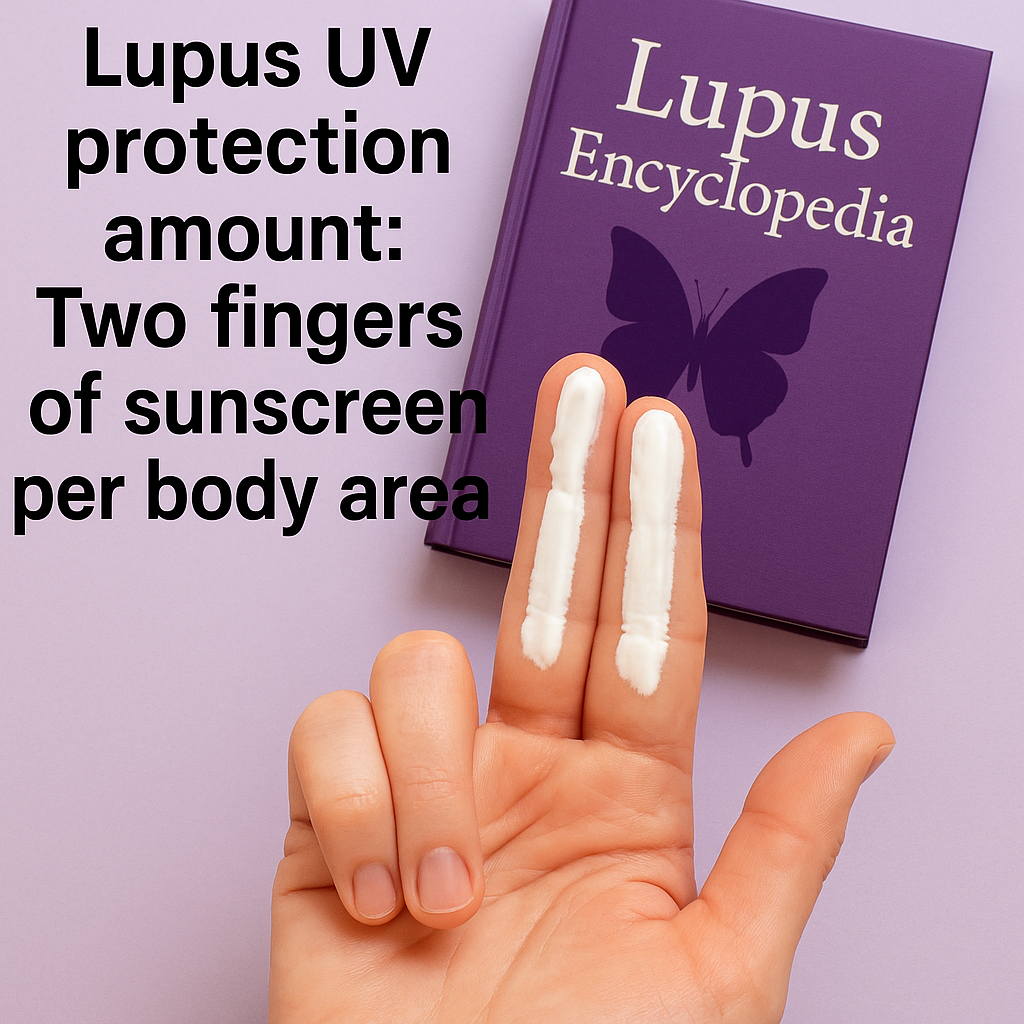
If you were recently diagnosed with lupus, it can be tough to find reliable, easy-to-understand information. Even if you were diagnosed a while ago, it can be a challenge. Click here, and I will tell you what I would do if I were diagnosed with lupus and give you advice on what you can do to improve your life. The Lupus Encyclopedia has lots of information for new, and not-so-new patients.